Every little girl dreams of being a princess. Fanciful hairstyling and tiaras, makeup and nail polish, glitter and hairspray ... and a glamorous princess gown!
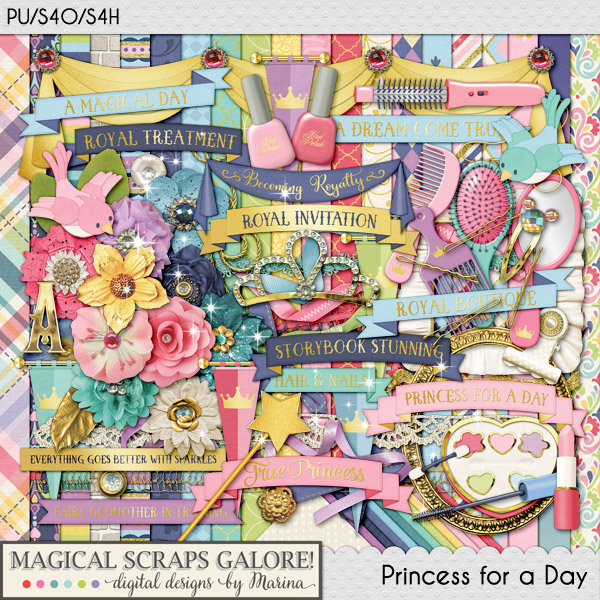
PRINCESS FOR A DAY by Magical Scraps Galore is a glamorous collection that will help you document your little girl's magical makeover into her favorite princess. Bursting with gorgeous girly colors and the perfect touch of sparkle and glitter, this collection includes beautiful elements such as hairbrushes and makeup, nail polish and lipstick, a tiara and a magic wand ... plus a full collection of Princess costumes, among many other fabulous goodies and patterns!
This is the perfect collection to document a Bibbidi Bobbidi appointment, a Princess meet and greet, a Princess birthday party, and so much more!
Find the full collection at 58% off -or the individual kit and add-ons at 30% off through Tuesday midnight at GingerScraps and The Digichick.


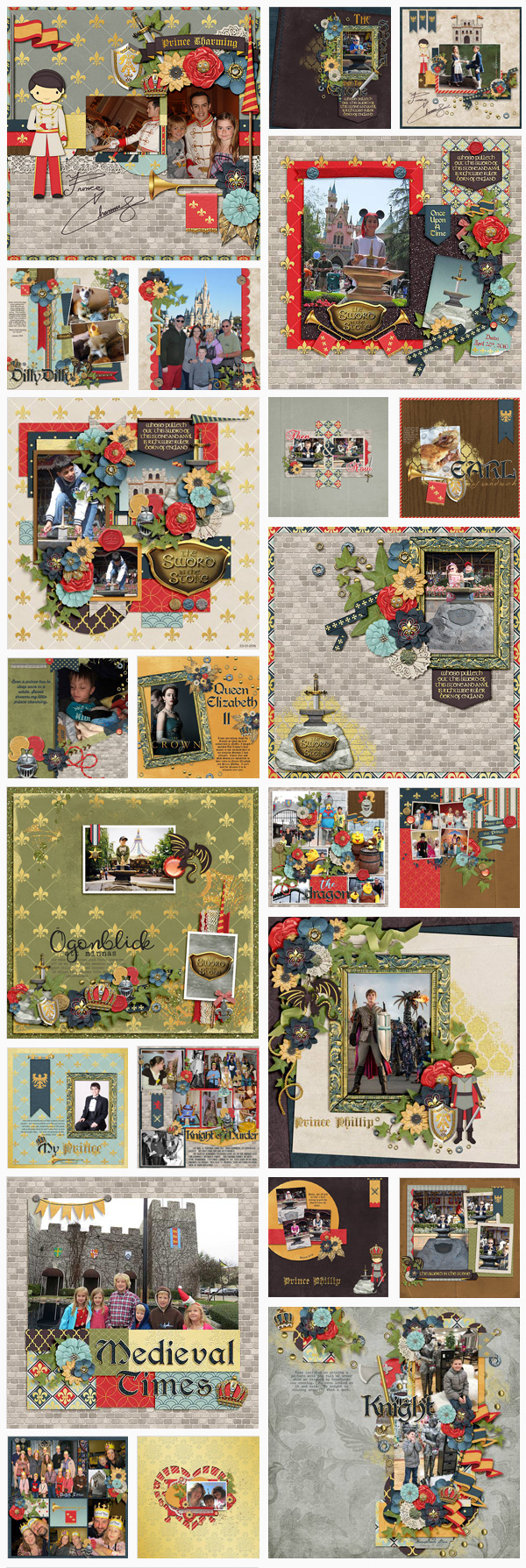
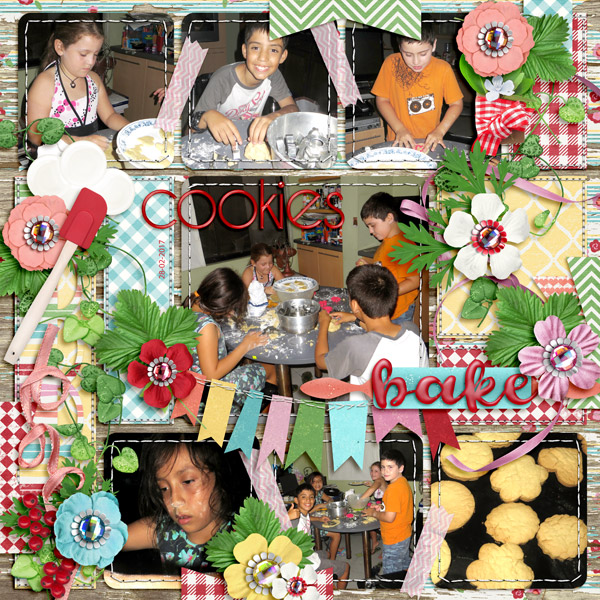
Some wonderful inspiration from the Creative Team:


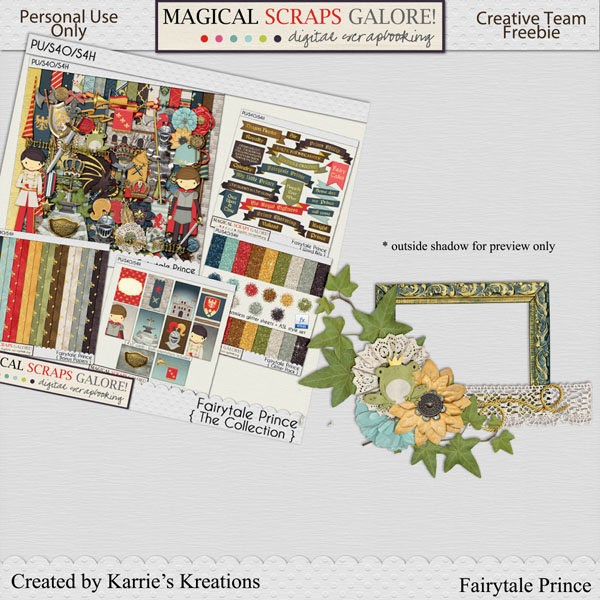
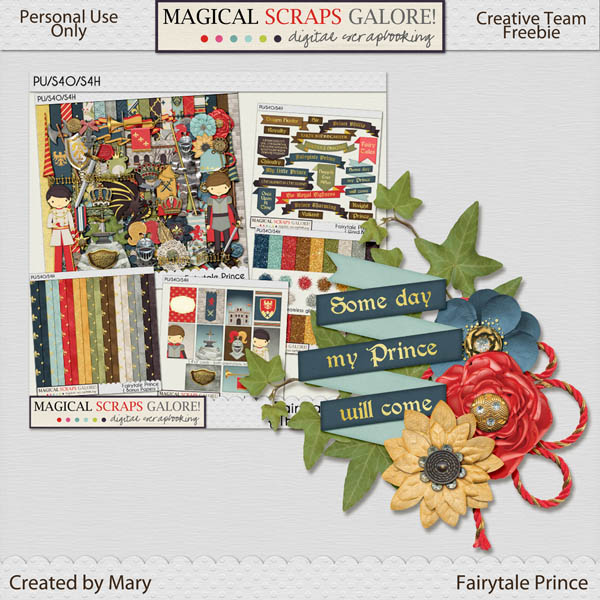
This week we have two gorgeous clusters to share, made by CT members Lisa and Karrie. Visit Marina's blog HERE to download and enjoy!:
Happy Scrappin Ya'All!